SUDEP
People who continue to have seizures are at greater risk of a number of complications, which is why preventing seizures and other problems is so important. The most serious complications are injuries and dying from seizures. This section gives frank information about one of the more common causes of dying from seizures called “Sudden Unexpected Death in Epilepsy,” which is abbreviated SUDEP.
What Is SUDEP?
SUDEP is the sudden, unexpected death of someone with epilepsy, who was otherwise healthy. In SUDEP cases, no other cause of death is found when an autopsy is done. Each year, more than 1 in 1,000 people with epilepsy die from SUDEP. This is the leading cause of death in people with uncontrolled seizures.
The person with epilepsy is often found dead in bed and doesn't appear to have had a convulsive seizure. Over one-third of the time, there is a witnessed seizure or signs of a recent seizure close to the time of death. They are often found lying face down. No one is sure about the cause of death in SUDEP and it may differ between cases. Some researchers think that a seizure causes an irregular heart rhythm. Other research has shown that breathing difficulties following a seizure lead to death.
Learn More:
Contact Our HelplineWhat Causes SUDEP?
No one knows what causes SUDEP, but many areas are being looked at. SUDEP occurs most often at night or during sleep when the death is not witnessed, leaving many questions unanswered. There may be evidence that a person had a seizure before dying, but this isn’t always the case.
Current research into the possible causes of SUDEP focuses on problems with breathing, heart rhythm and brain function that occur with a seizure.
- Breathing: A seizure typically may cause a person to briefly stop breathing (apnea). If these breathing pauses last too long, they can reduce the amount of oxygen that gets to the heart and the brain. A lack of oxygen can be life threatening if not treated immediately. Also, a person’s airway may sometimes get blocked blocked during a convulsive seizure, leading to suffocation (inability to breathe).
- Heart Rhythm: Rarely, a seizure may cause a dangerous heart rhythm or cardiac arrest.
- Brain Function Seizures may suppress or interfere with the function of vital areas in the brainstem. These areas are responsible for breathing and heart rate as well as other important body functions. As a result, changes in brain function could cause dangerous breathing and heart rate changes.
- Others: SUDEP may result from more than one cause, or from a combination of breathing difficulty, abnormal heart rhythm and changes in brain function. Or, it may result from factors researchers have yet to discover.
Can SUDEP Be Prevented?
Until further answers are available, the best way to prevent SUDEP is to lower your risk by controlling seizures. Research has found that people with all types of epilepsy that experience convulsive seizures can be at risk.
For most people living with epilepsy today, the disease can be controlled with available therapies and good seizure-management practices. For example, avoiding seizure triggers and working with and epilepsy specialist. And for people with the most severe types of difficult to control epilepsy, there are steps an individual can take to lower one’s risk, including:
- Epilepsy surgery
- Neurostimulation devices
- Dietary therapies
- Participating in research to find new, more effective therapies.
Learn how to get the best care and decrease your risk for SUDEP.
Learn More:
Support the SUDEP ProgramReducing the Risk of SUDEP
The best way to prevent SUDEP is to have as few seizures as possible.
- Get the best seizure control possible. This may involve actions such as:
- Taking medication regularly and at the right dose.
- Visiting your health care team regularly, especially if seizures are not controlled.
- If medicines do not work, consider other treatment options such as epilepsy surgery, devices, or dietary therapy.
- Take good care of yourself or your loved one. Eat well, get enough rest and regular exercise, avoid drinking too much alcohol or using recreational drugs, and minimize stress when possible.
- Be aware of and avoid any potential seizure triggers whenever possible. Keep a record of things that occurred before a seizure (such as illness, tiredness, stress, missing medications, and where and when the seizure occurred).
- Talk to your doctor about having your heart checked (cardiac evaluation) to rule out any heart problems. This is especially important if the diagnosis of epilepsy is not certain or the seizures are not controlled.
- Be seizure safe. Make sure family and co-workers know what to do for seizure first-aid, take extra precautions around water, including swimming and bathing.
Check out the #AimForZero Special Report that identifies four key actions to help reduce your risk of seizures.
Spotlight: Ketogenic Diet And SUDEP
Jeff Buchhalter, MD, PhD, talks about the ketogenic diet as a treatment for seizures and how its use might reduce the risk for SUDEP.
Frequently Asked Questions About SUDEP
How common is SUDEP?
- Each year, more than 1 in 1,000 people with epilepsy die from SUDEP.
- People with poorly controlled epilepsy are at greatest risk of dying from SUDEP.
- SUDEP takes more lives annually in the United States than sudden infant death syndrome (SIDS).
- People with only absence or myoclonic seizures are not known to have increased risk for sudden death.
Who is at risk for SUDEP?
The greatest risk factor for SUDEP is having tonic clonic seizures (grand mal).
People with night time seizures may also be at higher risk.
Missing medications or not taking seizure medicines as prescribed, because it can lead to more seizures, may also put people at higher risk for SUDEP.
Is my child at risk for SUDEP?
The answer depends on how severe the epilepsy is and the type of seizures she is having. While some studies found that rates of SUDEP are lower in children, others found rates similar to those seen in adults.
Is it SUDEP if there was no evidence of a seizure?
Often there are signs that a person had a seizure before dying, but this isn’t always the case. While a seizure is not a requirement for SUDEP to be diagnosed, recent studies suggest most SUDEP are likely seizure-related.
Is SUDEP genetic?
There are some studies that suggest genetic factors may play a role, but no definite information is available at this time. Several research efforts are looking into genetics and SUDEP. Read more about the Search for Genetic Risk Factors for SUDEP.
Should I talk to my doctor about SUDEP?
Yes! If your doctor has not spoken to you about the health risks associated with epilepsy, you should ask them about SUDEP.
Questions to ask may include:
- What risks do I or my family member have for SUDEP?
- What can we do to lessen the risk of SUDEP?
If I have lost a loved one to SUDEP, can I participate in research?
If you have recently lost a loved one to SUDEP, contact the North American SUDEP Registry (NASR) and participate in their study to help find the causes of SUDEP. The multicenter NASR provides clinical data, DNA and brain tissue for the scientific community to study. For more information call 855-432-8555 or email info@sudepregistry.org; or contact Dr. Devinsky at 646-558-0801 or email od4@nyu.edu.
The Ion Channels in Epilepsy study at Baylor College of Medicine is also accepting participants. This study is trying to identify genetic risk factors that may make a person with epilepsy more likely to die suddenly. For more information, contact Dr. Goldman at 713-798-0980 or email agoldman@bcm.edu.
More Information On SUDEP
- Talk to the physician or other health care professional treating your seizures about SUDEP.
- Get SUDEP Brochures and Materials.
- Download or watch the SUDEP presentations and webinars.
- Learn about current SUDEP Research efforts.
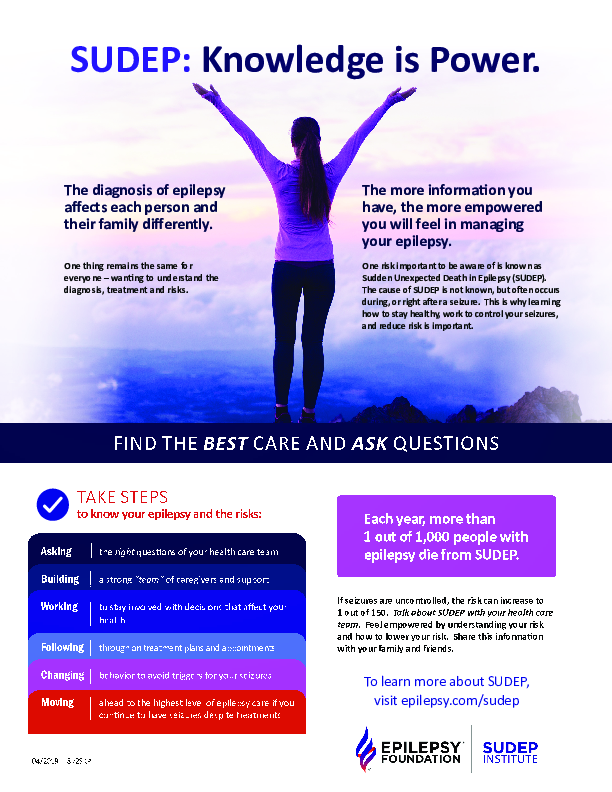
Knowledge Is Power
Download our "Knowledge is Power" flyer for help seeking the best care and knowing what questions to ask your health care provider about your SUDEP risk.
Get answers to frequently asked questions about SUDEP.
Learn about the SUDEP program
Sharing SUDEP Stories: eJourney
Share your SUDEP story with the world. Whether you are a family member, friend, or caregiver that has been impacted by SUDEP – your story matters. Sharing written stories, videos and photographs helps create understanding, support and increases awareness about SUDEP.
Through the power of eJourney, we can increase SUDEP awareness, help others to not feel so alone, and empower the community to help make a difference. Read eJourneys about SUDEP:
#StartTheSUDEPConvo Video Series
The Epilepsy Foundation has produced a video series to raise awareness about Sudden Unexpected Death in Epilepsy (SUDEP) and improve communication between patients and their healthcare providers. The videos honor the lives of those who have been lost to SUDEP and highlight stories of people who live with uncontrollable seizures and healthcare providers.
To roll out the videos, the Epilepsy Foundation will be implementing a digital media campaign called #StartTheSUDEPConvo to inspire people to discuss SUDEP, educate people with epilepsy and their caregivers about the risks for SUDEP, and help them manage their epilepsy. The Foundation is planning to upload one video a month on its eJourney Community Blog starting April 4 and leading to SUDEP Action Day on October 19.
These videos will also be shared on the Foundation’s social media channels, including Facebook, Twitter, Instagram, and LinkedIn. In addition to sharing the #StartTheSUDEPConvo videos, the Epilepsy Foundation will post monthly educational content about SUDEP.
SUDEP Resources
What Can I Do If I Have Lost A Loved One To SUDEP?
Please read our page on support for bereaved families. You will be able to learn about the programs and services available for families who have lost a loved one to SUDEP. In the meantime, please email sudep@efa.org or call 1-800-332-1000, and press option 1 to speak with an Information Specialist.
What Is The Epilepsy Foundation Doing To Prevent SUDEP?
To ensure that SUDEP gets the public awareness and research attention it deserves, the Epilepsy Foundation has launched the SUDEP program.
- Learn about the SUDEP program
- Learn about the SUDEP program's Biomarker Challenge
Additional Resources
- American Epilepsy Society
- Centers for Disease Control and Prevention
- Chelsea Hutchison Foundation
- Citizens United for Research in Epilepsy
- Danny Did Foundation
- FACES (Finding A Cure for Epilepsy and Seizures)
- Making Sense of SUDEP
- North American SUDEP Registry
- Partners Against Mortality in Epilepsy
- SUDEP Action
- SUDEP Aware
Learn More:
Find Your Local Epilepsy FoundationResources
Epilepsy Centers
Epilepsy centers provide you with a team of specialists to help you diagnose your epilepsy and explore treatment options.
Epilepsy Medication
Find in-depth information on anti-seizure medications so you know what to ask your doctor.
Epilepsy and Seizures 24/7 Helpline
Call our Epilepsy and Seizures 24/7 Helpline and talk with an epilepsy information specialist or submit a question online.
Tools & Resources
Get information, tips, and more to help you manage your epilepsy.